Frequently Asked Questions
Don’t speak fluent healthcare? We can translate. Find answers to frequently asked questions here.
FAQs
What is the Transparency in Coverage and No Surprises Act?
Refer to our overview here for details.
How do I add a physician to our practice?
Complete a Participating Provider Add Form and submit copies of the new physician’s Hawaii State and Federal DEA licenses (if applicable). Please include the provider group’s TIN (Tax ID Number) and NPI (National Provider Identifier) number(s).
Can I receive my reimbursements with an automatic deposit?
Yes. See the section on Electronic Funds Transfer (EFT).
How do I change my billing address?
Complete the Existing Provider Change form to report changes in billing address.
How often is the provider/physician fee schedule revised?
The provider/physician fee schedule is updated every two years, based on the prior year’s Medicare rates.
How do I report a change in company name and/or Federal Tax ID number?
Complete the Existing Provider Change form to report changes in company name and/or Federal Tax ID number, along with an updated W-9 form. If both have changed, please contact Customer Services as you may have to sign a new Provider Agreement.
My current Provider Identification Number (PIN) is my social security number. Can that be changed?
Yes. Send a request in writing and we will send you a new unique PIN number. Submit your request to:
UHA Contracting Services
700 Bishop Street, Suite 300
Honolulu, HI 96813-4100
Toll free fax: (866) 572-4383
Email: [email protected]
What is the patient co-pay for a physician office visit?
The patient’s UHA plan is listed on the member ID card. Currently the co-payments are:
UHA 3000 (Bundle): $12*
UHA One Plan℠ (Bundle): $12*
UHA 600 (Bundle): 10% of the eligible charge*
*Tax on the physician office visit charge is not a covered benefit. The provider is responsible for calculating the tax portion based on the eligible charge. Co-payment amounts are subject to change without notice.
Am I able to check claim status or claim payments online?
Online Claim status is now offered via Online Provider Services. For more information contact Customer Services at (808) 532-4000, or toll free at 1-800-458-4600 from the Neighbor Islands.
Are EDI claims submissions accepted?
Yes. There are two ways to submit EDI claim submissions. A connection can be made directly to UHA as an 837 transaction or through the Hawaii Xchange online service. Click here to read more about each submission method.
What is the procedure for submitting a claim, where Medicare is primary and UHA is secondary?
Submit the Medicare Explanation of Benefit along with the claim form to UHA.
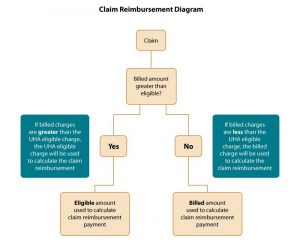
How do claims get paid based on billed charges?
Refer to the diagram below. Please contact Customer Services if you need further assistance.
Can a claim be reconsidered?
Yes, claims can be reconsidered for a variety of reasons. Please contact Customer Services for assistance.
What if I am still not satisfied with the final decision of my reconsidered claim?
If you are not satisfied with our response to your concern, and wish to pursue the matter further, you must appeal the decision by submitting a written appeal. The appeal must be filed within one year of the date UHA informed you of the denial or limitation of the claim or coverage for the requested service. Appeals must be submitted in writing to:
UHA Appeals Coordinator
700 Bishop Street, Suite 300
Honolulu, HI 96813
Your appeal will be reviewed by staff not involved in the original decision (nor a subordinate to the original decision maker). If the appeal concerns a clinical matter, it will be reviewed by an independent licensed practitioner with appropriate expertise and experience. If we need additional information to complete our review, we will notify you and give you reasonable time to respond.
For more information, please view our Provider Handbook.
The final decision will be made by the UHA Appeals Committee. You will be notified of the final decision within 60 days of receipt of your written appeal, or within 30 days if your appeal concerns a denial of a clinical matter.
Expedited Appeals
You may request an Expedited Appeal if the standard time (30 or 60 days, as set forth above) for completing an appeal would:
- seriously jeopardize the member’s life or health;
- seriously jeopardize the member’s ability to gain maximum functioning; or
- subject the member to severe pain that cannot be adequately managed without the care or treatment requested.
To request an Expedited Appeal, call Health Care Services.
What if I am still not satisfied with the final decision of my appeal?
If you wish to contest our decision on any appeal, you must agree to binding arbitration. To request binding arbitration, you must submit a written request for arbitration to UHA within 60 days of the date of the letter communicating the decision of the Appeals Committee. Both parties will agree on the person to serve as the independent arbitrator. The decision of the arbitrator is binding on both parties. Costs for the arbitration will be shared as ordered by the arbitrator. Further details are provided in your Participating Provider Agreement.
How do I refer a patient to a participating specialist?
Primary care physicians (PCP) and other participating specialists may direct members to any participating specialist. A formal referral is not necessary.
How do I refer a patient to a non-participating specialist?
Complete the Request for Authorization form or contact Health Care Services to discuss the referral.
Can another primary care provider (PCP) see my patient?
Yes. In order to meet the needs of our members, our plans allow for this kind of flexibility.
Is prior authorization required for mental health outpatient visits?
No.
Who is responsible for prior authorization for procedures performed by a specialist?
The specialist that will be performing the procedure is responsible for obtaining authorization by completing a Request for Authorization form. The primary care physician (PCP) should also be notified.
How are approved requests for authorization confirmed?
Providers who have registered for Online Provider Services* may view the status of authorization requests online. Otherwise, approved requests are confirmed in writing and delivered either by mail or fax. You must receive more than verbal notification for non-emergency care.
* For more information about Online Provider Services, please click here.
How long does it take to get an authorization approved?
We ask that you submit your prior authorization well in advance of the service date(s), allowing two weeks (15 days) for a determination to be made.
May I submit an expedited request for prior authorization?
You may, but be aware that expedited requests are defined as those which may seriously jeopardize life or health, or the ability to regain maximum functioning.
May I submit a request for authorization after a procedure has been performed?
Not typically, but requests will be handled on a case-by-case basis. Complete a Request for Authorization form and submit it for consideration.
Tip #1: How to Avoid Returned Claims
Reduce the time it takes to process your claim and avoid a returned claim by completely and correctly filling in the claim form.
The following items, if missing or incorrect, will delay processing of your claim or even result in a request for re-submission:
- Subscriber’s name
- Subscriber’s member ID number (11-digits)
- Patient’s name and date of birth
- Date of service
- UHA group number (4-digits)
- Name of referring physician for claims from laboratories, radiologists, and consultants
- Date, place, and cause of injury
- Descriptive diagnosis and ICD-9 code
- Descriptive procedures and CPT code
- Charges
- Provider’s billing name and address
- Provider or agent’s signature
- Supportive data for modifiers, e.g. after-hours modifier – claim should have time listed
- Provider Identification Number (PIN)
- Federal tax ID number
Tip #2: Coding Corner
Avoid the following possible claims(s) denials:
- Claim submitted with Modifier -25 or -57?*
- Tip: Submit your claims with supporting documentation indicating a significant, separately identifiable evaluation and management service by the same physician on the same day of the procedure or other service.
- Claim submitted with Modifier -59?*
- Tip: Submit your claim with supporting documentation indicating the service was distinct or independent from other service(s) performed on the same day.
- Claim submitted with duplicate CPT codes?*
- Tip: Submit your claim with supporting documentation indicating the service(s) is not a duplicate.
- UHA is secondary insurance carrier?*
- Tip: Submit your claim with primary insurance carrier’s EOB (Explanation of Benefits)/RA (Remittance Advice).
*You may also apply this information for previously denied claims resubmitted for reimbursement reconsideration
Tip #3: How to Complete the CMS-1500 Claim Form
Box 21 – DIAGNOSIS OR NATURE OF ILLNESS OR INJURY – ICD INDICATOR
Use the ICD-9 or ICD-10 code for each current diagnosis applicable to that visit. Do not put any description for each diagnosis code. The new form requires that codes be entered in the correct order following the alphabetical reference numbers (A-L) codes are entered left to right (alphabetical order), 4 codes per row, and up to 3 rows. NOTE: This is different from the old CMS form where only up to 4 codes can be entered and according to the numerical order.

UHA recommends that the diagnosis reference numbers (A-L) be used in COLUMN 24E to correspond with the services.
“ICD IND” Use this space to indicate if the diagnosis codes being used are ICD-9 or ICD-10 codes. An indicator of “9” would represent ICD-9 codes and a “0” indicator would represent ICD-10. This is a required field.
Please contact Customer Services if you require assistance.
Tip #1: Common Reasons for Claim Denials
Here are three common reasons a claim may be denied and some helpful tips to get your claims paid without delay:
- Denial Reason: “Duplicate claim”:
- Check other claims to see if the service was paid on another claim;
- If the service in question was not paid on another claim:
- Do NOT resubmit the same claim.
- Instead, submit the Provider Claims Action Request form with clinical notes.
- Denial Reason: “Exceeded timely filing”:
- Submit the Timely Claim Filing Waiver Form for providers with supporting documentation.
- Denial Reason: “No Prior Authorization on file”:
- Submit the Prior Authorization Request Form for appropriate services with clinical notes for retroactive review:
- Reference list of Services That Require Prior Authorization
Tip #2: Timely Filing Waivers
Acceptable reasons for timely filing waivers:
- Claim submission within 12 months from date of service
- Claim submission within 12 months from date of denial
- Claim submission within 12 months from newborn enrollment
- Claim submission within 12 months from primary carrier’s payments
- Claim submission within 12 months of third party liability payer exhaust denial (must provide dated denial)
If none of the above reasons apply, a Claim Filing Waiver Form may be submitted with one of the following documents that support attempts of earlier claims submissions:
- Copy of the electronic claim denial/rejection notification
- Dated correspondence from UHA with claim information detailing why claim was rejected
- Dated confirmation of claim receipt
When requesting a waiver, please use the Timely Claim Filing Waiver Form.
If you have any questions regarding timely filing, please contact Customer Services at (808) 532-4000, extension 351, from Oahu or (800) 458-4600, extension 351, from the neighbor islands.
Tip #3: Resubmissions, Corrections, and Reconsiderations
- What should you do if you are asked to resubmit a claim with notes?
- Submit a paper claim with medical notes attached and write “Resubmission” at the top right hand corner.
- What should you do if there is a denial on your claim that you disagree with?
- Complete and submit a “Claim Reconsideration Request” form along with your medical notes.
- Do not submit a claim with the “Claim Reconsideration Request” form to avoid a duplicate claim denial.
- What should you do if you would like to make a correction on a previously submitted claim?
- Submit a paper claim and write the words “Corrected Claim” at the top right hand corner.
- Please ensure that the corrected claim matches your original claim with the exception of the area(s) that is being corrected.See example below:
Original Claim

Corrected Claim

(Line 1: CPT changed to 99213 / Lines 2 & 3 identical to original claim)
What is UHA's Pharmacy Benefits Management Company?
UHA switched over to Express Scripts as of June 1, 2016 in response to customer feedback and our desire to rein in the skyrocketing costs of prescription drugs. In order for UHA to care for the needs of our members, we have to align ourselves with partners who will be able to help us curb costs. Because of its size and position in the industry, Express Scripts offers more competitive pricing and service for our members.
What is CareContinuum?
Some medications, such as injectables, infusions, and some specialty drugs are part of a member’s medical benefit rather than the pharmacy benefit. Express Scripts not only manages our pharmacy benefits for our members (PBM), but through their company CareContinuum, they can also manage medications under the member’s medical benefits (MBM). There is a MBM v. PBM Drug Lookup tool available here.
Where can pharmacists call for claims processing questions?
Pharmacists can call the Pharmacy Help desk at (800) 922-1557 to assist with claims processing for medications managed under the member’s pharmacy benefit (PBM) at any time of the day or night.
For help with claims processed according to the member’s medical benefit (MBM), pharmacists can call UHA Customer Services, Monday – Friday, 8am to 5pm Hawaii Standard Time, at (808) 532-4000, Toll free: (800) 458-4600.
What drugs are excluded?
Please see the list of excluded medications and their alternatives: Express Scripts.
My patient just changed plans to UHA. How will I know if my patient’s prescription medications require a prior authorization, if they are non-covered, or if they are non-preferred under their drug coverage?
We recommend that you visit uhahealth.com/express-scripts to see if there will be changes to the coverage of your patient’s medications:
- Which medications are included in our Formulary and which medications will require PA, step therapy, or have a quantity limit
- Which medications will not be covered
How do I enter PA requests for my patient's medications?
For fastest service visit Express Scripts’ provider portal at www.evicore.com/provider.
- This one-stop site will allow you to submit PA requests for medications managed under the member’s pharmacy benefit (PBM) and those managed under the medical benefit (MBM). In most cases you will be able to receive a real-time response. You can also set up email notifications which will send updates either on a daily basis, or if you prefer, only when a decision has been made.
- PA requests for medications that are managed under the member’s pharmacy benefit may also be submitted via covermymeds.
- Physicians may also call in PA requests for medications managed under the member’s pharmacy benefit (PBM) at any time of the day or night. And in most cases, you will get a real-time response.
- PBM Phone: (800) 753-2851
- PBM Fax: (877) 251-5896
- For PA requests for medications managed under the member’s medical benefit, call CareContinuum, the plan’s Medical Benefit Manager (MBM), Monday – Friday, 8am to 10pm Eastern Standard Time. Messages received after business hours will be returned the next business day.
- MBM Phone: (866) 877-7042 (Press Option #1 for PA questions)
- MBM Fax: (866) 877-7179
How can pharmacists check on PA status for patients prior to administering or dispensing?
Pharmacists may call the MBM or PBM phone number to obtain status on PA’s or check with the provider’s office who submitted the PA. The Pharmacy can register at www.evicore.com/provider also and submit PA’s. They can receive email notifications of status on a daily basis, or just when the decision has been made. Once ESI approves a PA, they will fax a notification to both the prescribing physician and the pharmacy listed on the PA.
- PBM Phone: (800) 753–2851
- MBM Phone: (866) 877-7042
How do I know which medications are managed under the member's medical benefit (MBM) and which are under the pharmacy benefit (PBM)?
Many injectable, infusion and specialty medications are managed under the member’s MBM rather than the PBM. Submitting PA requests via evicore.com portal eliminates the need to differentiate between the two. PA requests for drugs managed as a medical benefit or as a pharmacy benefit may both be submitted on the same user friendly website www.evicore.com/provider.
If you choose a different submission method, you can find out which medications are managed by the member’s medical benefit (MBM), and which are managed by the member’s pharmacy benefit (PBM) by using the MBM v. PBM Drug Lookup tool available on the Drug Search for Providers tab of the Find Care Providers & Drugs page.
What are UHA’s utilization management requirements?
These clinical programs protect your patient’s health and save them money: step therapy (ST), drug quantity management (QL) and prior authorization (PA):
Step Therapy
- Step therapy is a program for patients who take prescription medicine regularly to treat a long-term condition, such as arthritis, asthma or high blood pressure. It lets patients get the treatment they need affordably. It helps the plan sponsor maintain prescription-drug coverage for everyone the plan covers. In step therapy, medicines are grouped in categories based on treatment and cost.
- First-line medicines are the first step. First-line medicines are generic and lower-cost brand-name medicines approved by the U.S. Food & Drug Administration (FDA). They are proven to be safe, effective and affordable. Step therapy suggests that patients should try these medicines first because in most cases they provide the same health benefit as more expensive drugs, but at a lower cost.
- Second-line drugs are the second and third steps. Second-line drugs typically are brand-name drugs. They are best suited for the few patients who don’t respond to first-line medicines. Second-line drugs are the most expensive options.
- Members who are currently taking a second line drug will not be asked to switch to a first line drug. They will be grandfathered indefinitely.
- If you prescribe a new medication for a patient with a step therapy requirement, they will be asked to try a first-line medication before a second-line medication.
Drug Quantity Management
- The drug quantity management program makes sure that patients are getting the right amount of medication and that is prescribed in the least wasteful way. For example, you instruct your patient to take two 20mg pills each morning. If that medication was also available in 40mg pills, we would reach out to you about prescribing one 40mg pill a day instead of two 20mg pills. In addition, if you wrote the original prescription for 30 pills (a 15-day supply), the new prescription for 30 pills would last a full month — and the patient would have just one copayment, not two.
- This program also makes sure that the prescription doesn’t exceed the amount of medication that the plan covers. If the prescription is for too large a quantity, the pharmacist can fill the prescription for the amount that the plan covers or contact you to discuss other options, such as increasing to a higher strength or getting a prior authorization for the quantity originally prescribed.
Prior Authorization
- When a prescription requires prior authorization, you can submit a PA request to Express Scripts or prescribe a different medication that is covered by the plan.
How do I register for the eviCore.com portal?
Registration is quick and easy! Visit myevicoreportal.medsolutions.com/User/Registration/Index.
You can register with only 6 simple steps and log in right away to begin submitting PA’s online. A tutorial can be found here.
As a provider who submits prior authorizations, is there training information available for my staff to learn how to submit PAs?
Please see the evicore.com Web Portal Overview for step by step illustrations.
Where are the PA forms for medications?
With electronic prior authorization, spend more time with patients and less time faxing. Visit www.evicore.com/provider to submit PA requests any time day or night and in most cases receive a response right away.
How do I request an expedited review?
Using the online PA portal, www.evicore.com/provider, or submitting your PA via phone, is the fastest way to receive a response. In most cases you will receive a real-time answer, and if approved, the patient will be able to pick up their medications right away.
What if I want to appeal a decision made by Express Scripts?
If you disagree with a decision reviewed under the member’s pharmacy benefit (PBM), you may contact UHA’s Health Care Service Department Monday-Friday from 8am to 5pm HST to request a peer-to-peer conversation within 30 days of the denial. We will arrange a time for you to speak with our Medical Director or Chief Medical Officer to discuss reconsideration. If you would like to submit a formal, written appeal to UHA, please follow our appeals process described here.
If you disagree with a decision made by CareContinuum (MBM), please contact them at (866) 877-7042, Monday-Friday: 8am-10pm EST. With CareContinuum you will be able to request a peer-to-peer or submit a formal written appeal.
Do I have to call Express Scripts, or can I call UHA's customer service line?
Express Scripts can answer your questions quickly and accurately around the clock for questions about drugs managed under the member’s pharmacy benefit (PBM). For medications managed under the member’s medical benefit (MBM), any calls received outside of business hours will be returned the next business day.
UHA’s phone lines are also available from 8am to 5pm, Monday through Friday, except for major holidays. A representative can be reached at: 808-532-4000 (or 800-458-4600 from the neighbor islands) at the following extensions:
- Customer Services: ext. 297
- Health Care Services: ext. 300
- Employer Services: ext. 299
- Premium Billing: ext. 353
Express Scripts Contact Information
PBM:
- Member Customer Service: Specific number for member inquiries; listed on the back of the member ID cards.
Phone: (855) 891-7978
Available 24/7 - Prior Authorizations: Contact for physicians to call or fax in PHARMACY prior authorizations.
Phone: (800) 753 – 2851
Fax: (877) 251-5896
Available 24/7 - Pharmacy Help Desk: For pharmacy use only to assist with getting a claim to adjudicate or understanding a reject message.
Phone: (800) 922-1557
Available 24/7 - TDD: Member Customer Service number for hearing impaired members.
Phone: (800) 759-1089
Available 24/7
MBM:
- Prior Authorizations: Contact for physicians to call or fax in MEDICAL drug prior authorizations.
Phone: (866) 877-7042
Fax: (866) 877-7179
Mon – Fri 8AM – 10PM (EST), 2AM – 4PM (HST)
The forms and documents on this page require the free Adobe Acrobat Reader. Please download Adobe Reader.
